Endoscopic Spine Surgery
June 24, 2020
Sciatica
June 24, 2020Don’t Slumber Over That Lumber
Panchkula: Low back pain is a very common complaint and most people experience backache at some time or another in their lifetime. Fortunately, approximately 90% of episodes of low back pain are self-limiting and resolve within approximately six weeks, regardless of treatment. Lumbar spondylitis or lumbar disc disease is one of the most common causes of low backache. This is because the lumbar region bears the brunt of the body’s weight.
Lumbar spondylitis refers to a collection of degenerative disorders. The intervertebral disc acts as a shock absorber of the spine. It consists of the fibro-cartilaginous annulus fibrosus, surrounding the soft jelly-like nucleus pulposus, with aging, there is degeneration of the vertebrae and the disc causing bony osteophytes and internal disc disruption. This in turn could cause neural foramen or spinal canal narrowing. It has increasingly been recognized that along with compression, the release of aspecific inflammatory mediators of this pain, called tumor necrosis factor-alpha (TNF) is responsible for chemical radiculitis and pain.
Lumbar spondylitis can begin in persons as young as 20 years. It increases with, and perhaps is an inevitable concomitant of, age. It may affect about 27-37% of the population. There is an 80% incidence in individuals more than 40years. Despite this, only about 3-5% of individuals experience sciatica in their life. Most disc prolapses occur when a person is in their thirties or forties when the nucleus pulposus is still a gelatin-like substance. After age 50 or 60, lumbar spondylitis or spinal stenosis are more likely causes of low back pain or leg pain.
Three sets of problems are commonly seen in the lumbar spine,
> Lumbar disc prolapse.
> Lumbarcanal stenosis
> Lumbar spine instability.
Causes: Disc herniations can result in from general wear and tear, such as when performing jobs that require constant sitting. However, prolapse often results from jobs that require lifting or straining. The intradiscal pressure rises and the jelly-like nucleus pulpous strains out through the thin membrane,
There is also a strong genetic component.
Symptoms of disc prolapse: These can vary depending on the location of the herniation and the type of soft tissue/nerve affected. Segmental symptoms are caused by local disruption of the anatomy. The patient may have low back pain and/or pain extending to the buttocks. Neural symptoms are due to compression or irritation of the nerve root adjacent to the disc. It may be characterized as shooting or stabbing pain. Higher herniations(third or fourth lumbar levels) can radiate into the groin or anterior thigh.
Lowerradiculopathies (first sacral level) cause pain in the calf and bottom of the foot. The fifth lumbar radiculopathy, which occurs most commonly, causes lateral and anterior thigh and leg pain. Often, accompanying numbness or tingling occurs with a distribution similar to the pain. There might be accompanying muscle weakness.
On examination, patients may be neurologically normal, may have profound radiculopathy, or may even demonstrate a cauda equine syndrome. A positive straight-leg raising sign may be present. The back may appear scoliotic. Gait is often abnormal. Muscle weakness may be revealed particularly when testing walking on heels and toes.
Symptoms of lumbar canal stenosis
Patients may present with neurogenic claudication. These patients may have pain and numbness in both the lower limbs. At some point in the evaluation, tests may be performed to confirm or rule out other causes of symptoms such as spondylolisthesis, degeneration tumors, metastases, and space-occupying lesions, as well as to evaluate the efficacy of potential treatments options.
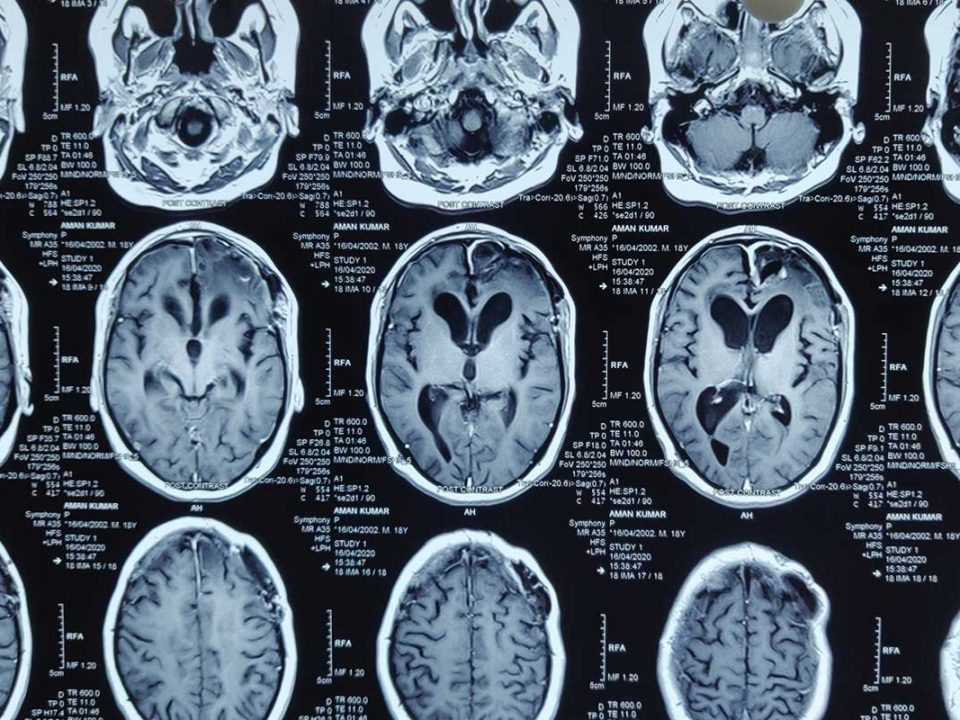
Magnetic resonance imaging (MRI) is the investigation of choice. It shows the anatomy of the tissue along with the nature of disc prolapse. X-rays give some indication of degenerative disc disease with signs such as narrowing of disc space, straightening of the spine. It also shows a grade of spondylolisthesis. It is also very essential to rule out diabetic neuropathy and other neurological conditions.
The majority of herniated discs will heal themselves in about six weeks and do not require surgery. Any patient having severe backache and radiculopathy may be advised bed rest for 10-12 days. Once pain and spasm decrease, patients can be initiated into physical therapy.
Medical treatment for lumbar disc disease is typically limited to providing a structured program of physical therapy and medications. Non-steroidal anti-inflammatory medications (NSAIDs), from the first line of treatment. One may consider drugs like ibuprofen or naproxen.
These medications can help relieve both the pain and inflammation associated with lumbar disc disease. Muscle relaxants, such as Cyclobenzaprine, Methocarbamol, Tizanidine Dantrolene can provide short-term relief for many people.
Antidepressants or drugs like Gabapentin are used in patients with radiculopathy.
A short course of oral corticosteroids, such as prednisone, can also be of benefit, but long-term use of corticosteroids is not recommended. For lumbar disc disease that causes severe, radiating nerve pain down the leg, epidural injection of corticosteroids may be considered to provide a more prompt anti-inflammatory effect.
The efficacy of epidural steroid injections is now generally thought to be limited to short term pain relief in selected patients only. Also, epidural steroid injections, in certain settings, may result from serious complications. Many people with lumbar disc disease can benefit from a structured program of physical therapy. This can assist with both strengthening of the abdominal and lower back muscles as well as overall conditioning of the body. They can be taught specific exercises that can be continued at home after the organized therapy program is completed. Other physical therapy modalities like heat therapy, electrical stimulation of muscles, ultrasound therapy can be applied.
Surgery:-
At times and situations, the indications for surgical treatment of symptomatic lumbar disc disease are not delineated. Nevertheless, situations exist in which most spine surgeons would probably agree with nonoperative intervention. These situations include the following:-
- A patient with cauda equina syndrome
- A patient demonstrating progressive neurologic deficit during a period of observation
- A patient with persistent bothersome sciatica pain, despite conservative management, for 6-12 weeks(at the period that varies from surgeon to surgeon)
What constitutes surgical therapy is open to discussion. Many choices are depending on the choice, the experience of the surgeon. The type of surgery would also be decided by the nature of the pathology. In all the procedures, the aim is to remove the disc and cause adequate nerve decompression. Out of all the procedures, microdiscectomy and especially endoscopic discectomy cause the minimum tissue damage.
The overall complication rate is 2-4% for the surgery. Infection, usually skin infection can occur. Very rarely, postoperative discitis can cripple a patient who is recovering.
Approximately 75% of patients who undergo a microdiscectomy have a long-term reduction of sciatic pain and, thus. Are considered cured.
The predominance of leg pain is the best determinant of a good outcome from surgery for lumbar disc herniation Interestingly, a 2006large multicenter trial found that surgical and nonsurgical outcomes at 2 years were similar, but that the surgical group experienced faster pain relief.
Conclusion
Small disc with or without symptoms and the medium-size disc with mild to moderate symptoms should be managed conservatively. Ono may consider surgery for medium size disc with severe symptoms. Large disc with or without neurological symptoms requires surgery. In a prolapsed disc, minimal tissue disturbance is desirable and so microdiscectomy arid endoscopic discectomy would be the procedure of choice.